Septal Perforation Repair: My Approach
Septal perforations — holes in the cartilage and tissue that divide the nose — can cause a wide range of symptoms that impact both comfort and quality of life. Some patients experience whistling, crusting, bleeding, or dryness. Others develop nasal obstruction, difficulty breathing, or even cosmetic changes to the nose over time.
Many people don’t realize that septal perforation repair is possible, or that it can often be performed at the same time as a rhinoplasty. The key is using a reliable technique that restores structure and stability.
In my practice, I repair septal perforations using a temporalis fascia graft combined with a PDS plate, a technique that has proven extremely effective for both small and large perforations — including those up to 2.5 cm or more in diameter.
My success rate with this method is over 90%, and this approach allows me to address both function and aesthetics during the same operation.
What Is a Septal Perforation?
A septal perforation is a hole in the nasal septum — the wall of cartilage and mucosa that separates the two nasal passages.
Common symptoms include:
whistling when breathing
crusting
bleeding
dryness
chronic irritation
nasal obstruction
decreased airflow
recurrent infections
saddle nose deformity (in advanced cases)
Common causes include:
prior septoplasty or rhinoplasty
trauma
chronic nasal picking
infection
autoimmune conditions
previous cautery
intranasal drug use
Not all perforations need repair, but those causing symptoms often benefit significantly.
Why Perforation Repair Is Challenging
Closing a septal perforation was difficult in the past because the tissue around the hole has reduced blood supply. Repairs fail when grafts or flaps don’t get enough vascular support. PDS plate and fascia simplified the repair and made it more predictable.
The goal of any successful repair is to:
recreate mucosal lining on both sides
restore structural separation
promote robust healing
stabilize the septum long-term
prevent recurrent breakdown
This is why I use a technique that reinforces both sides of the perforation and provides a scaffold for new tissue to grow across the defect.
My Preferred Method: Temporalis Fascia + PDS Plate
This is the technique I use because it is stable, predictable, and highly successful — even in larger perforations.
What each component does:
🟦 Temporalis fascia
This is a thin, vascularized tissue layer taken from a small incision above the ear.
It is:
strong
flexible
highly biocompatible
ideal for lining the septum
Temporalis fascia is frequently used in ear and nasal reconstruction because it integrates beautifully with surrounding tissue.
🟪 PDS Plate
PDS (polydioxanone) is a dissolvable material that acts as a structural scaffold.
When paired with fascia, it:
provides strength
stabilizes the repair
maintains the contour
supports mucosal regeneration
dissolves over months as healing completes
The combination allows the body’s tissues to grow across the perforation in a tension-free, stable environment.
What Size Perforations Can I Repair?
Using this method, I am routinely able to close perforations up to 2.5 cm or larger, depending on:
mucosal quality
blood supply
whether the patient is undergoing rhinoplasty simultaneously
presence of inflammation or crusting
structural integrity of surrounding cartilage
Larger perforations require careful planning, but they can be successful when properly supported.
Can This Be Performed During Rhinoplasty?
Yes — and this is one of the most valuable parts of this technique.
When combined with rhinoplasty:
I can restore structure
improve breathing
reinforce the septum
support the tip
correct functional issues
enhance aesthetics in the same operation
Septal perforation repair adds approximately one additional hour to rhinoplasty surgery, depending on the size and complexity.
Success Rate
Using this approach, my success rate is greater than 90%, which is significantly higher than many traditional mucosal flap techniques alone.
Key reasons for the high success rate:
double-layered repair
strong structural scaffold
excellent tissue integration
controlled environment during rhinoplasty
improved blood supply after correcting septal deviations
careful postoperative management
What Patients Can Expect After Perforation Repair
Recovery includes:
nasal splints (temporary)
saline sprays
humidification
avoiding trauma or nose blowing
follow-up visits to monitor healing
Most patients experience a significant reduction or complete resolution of their symptoms once the perforation heals.
Who Is a Good Candidate?
You may benefit from perforation repair if you have:
breathing difficulties
crusting or dryness
bleeding
whistling
nasal obstruction
structural weakness
visible deformity
discomfort
perforation discovered during evaluation for rhinoplasty
Not all perforations require closure, but symptomatic ones often do.
Why Technique Selection Matters
Many perforation repairs fail because:
the grafts are not supported
the tissues are under tension
blood supply is inadequate
the repair is too thin or fragile
Temporalis fascia + PDS plate provides:
strength
vascular integration
stability
long-term durability
It’s one of the most reliable methods for closing larger defects.
Bottom Line
Septal perforations can cause frustrating symptoms — but modern techniques have made closure consistently successful. Using a combination of temporalis fascia and a PDS plate, I’m able to repair perforations up to 2.5 cm+ with a success rate over 90%, often performed safely during rhinoplasty.
If you’re considering rhinoplasty or dealing with a septal perforation, there are excellent treatment options available, and a carefully planned structural repair can dramatically improve both function and quality of life.
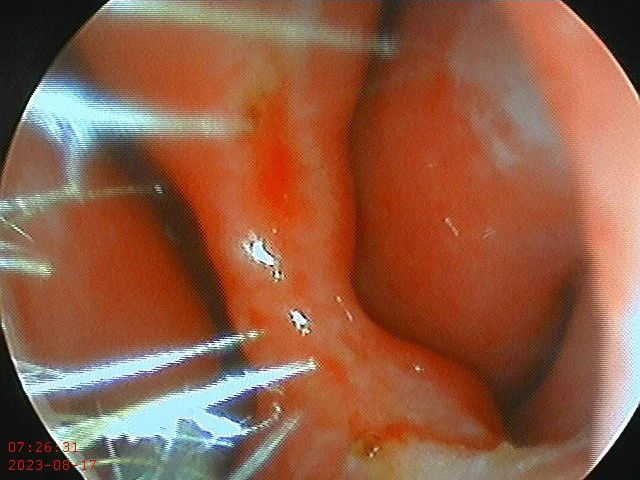
Perforation prior to repair
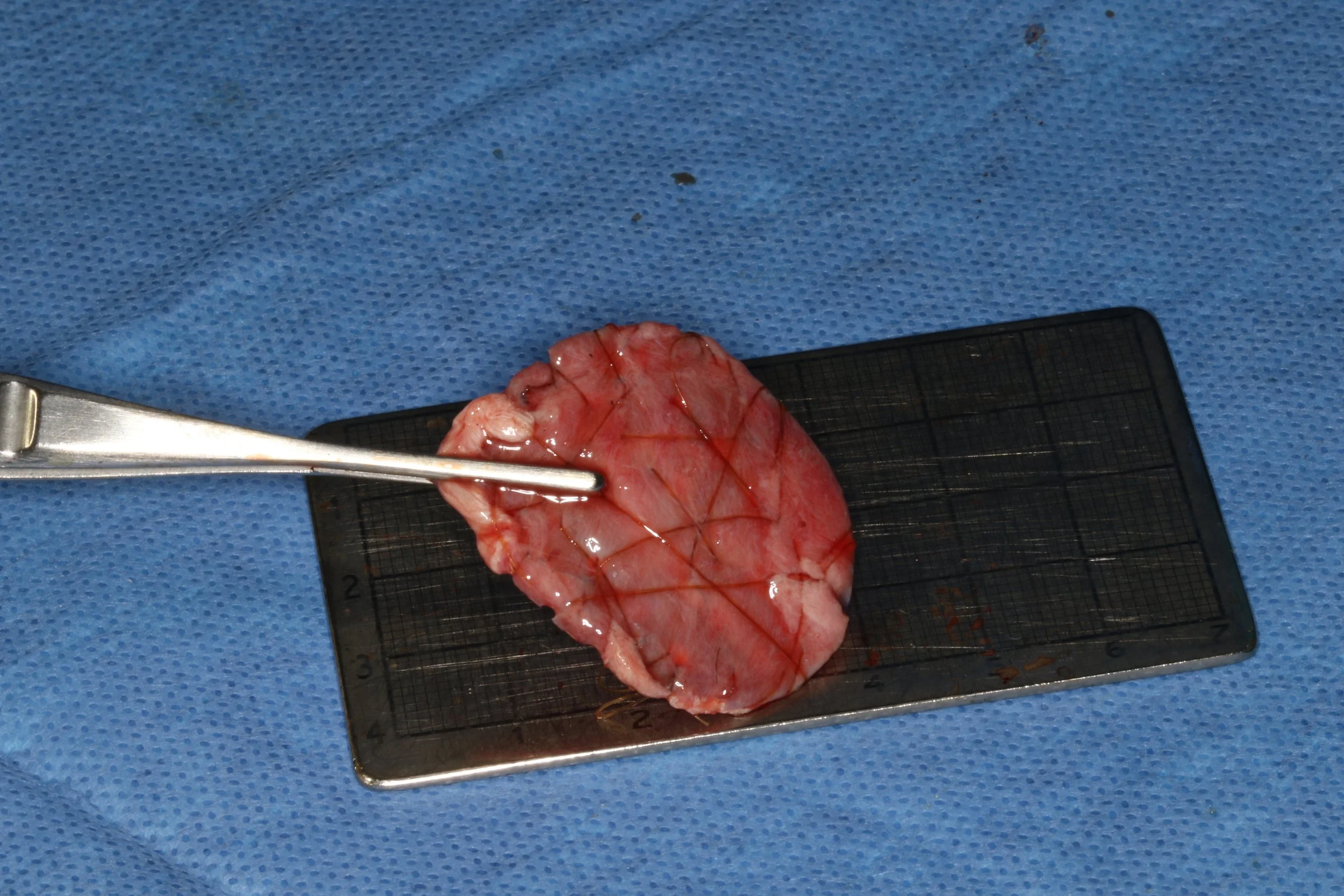
Temporalis fascia/PDS plate construct
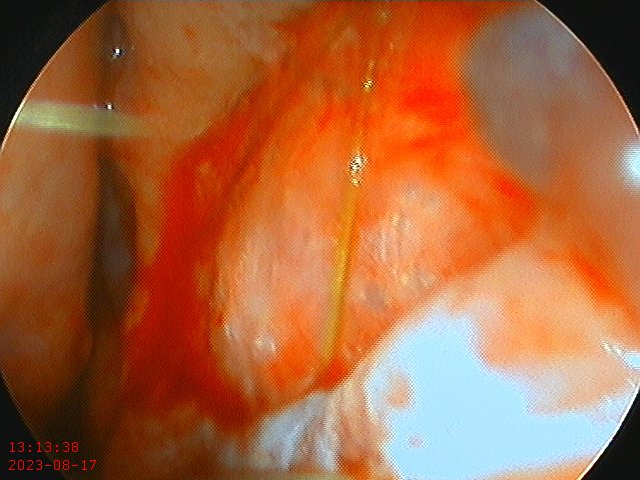
Fascia/Pds plate within the perforation closing a large, 2.5 cm perforation.